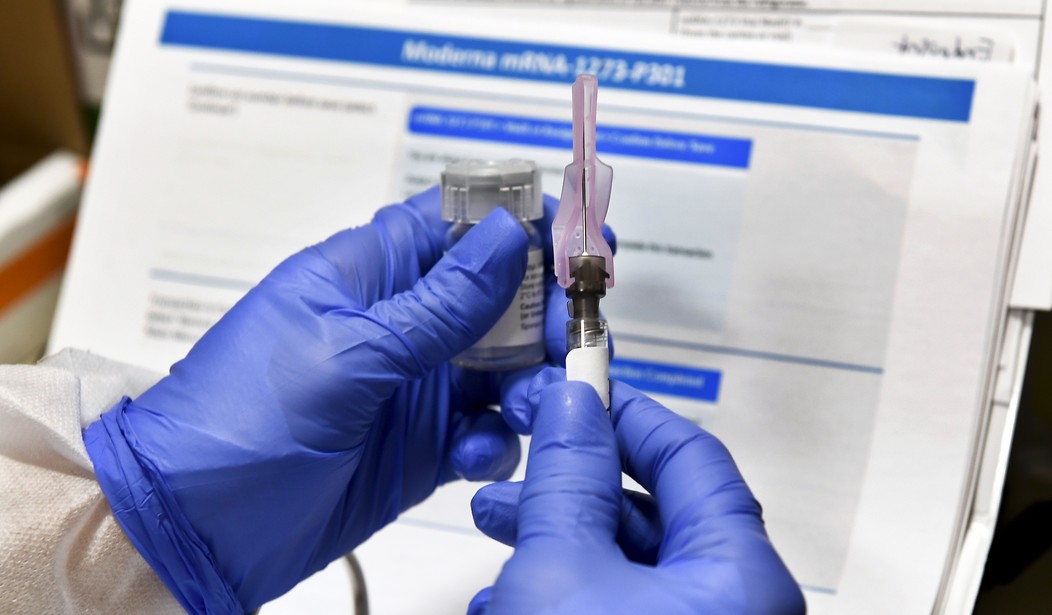
Thanks to the hard work of countless scientists, tens of thousands of trial volunteers, and yes, investors, the world is now on the cusp of curing COVID-19. The Pfizer and Moderna vaccines each boast around 95 percent efficacy and their approval is the key to ending endless lockdowns. There’s just one problem: regulatory foot-dragging. Despite United Kingdom (U.K.) regulatory authorities greenlighting the Pfizer vaccine, the Food and Drug Administration (FDA) insists on additional scrutiny while thousands continue to die from the deadly disease. While the American people deserve a robust approval process that takes all the evidence into account, the FDA's regulatory delay is compromising public health. It’s time for a cure to end this regulatory nightmare.
By now, the Pfizer and Moderna vaccines are old news. The FDA had previously stated that it will approve a vaccine with at least 50 percent efficacy, and now, the agency has admitted that the vaccine is “highly effective” in preventing confirmed cases of COVID-19 as soon as seven days after the second dose. The FDA’s advisory committee was able to vouch for the evidence and the head of the panel has predicted that the vaccine will be approved. The green light for mass inoculation could happen as early as December 12. This will mean that, at best, the FDA will approve Pfizer’s vaccine 10 days after the U.K. okayed the vaccine. The delay is a predictable result of differences in the regulatory philosophies of the two Western nations. While the U.K. leans more heavily on the exhaustive scientific research conducted by scientists in the private sector, the U.S. insists on double-checking these companies’ work. With daily COVID-19 deaths in the U.S. averaging more than 2,000 since around Thanksgiving, each day of delay costs thousands of lives.
The FDA is hardly in the best position to weigh hypothetical vaccine harms against the very real human costs caused by delays. For example, despite ample scientific evidence that tobacco harm reduction products such as vapes are 95 percent safer than cigarettes, the regulatory agency has a horrendous track-record in embracing these new technologies. Despite hundreds of scientific studies attesting to the efficacy of reduced-risk alternatives to cigarettes, the FDA continues to insist on wanton vaping regulation and arbitrary product removals. While it may seem surprising that scientists at the FDA aren’t keen on embracing evidence, such counterproductive policy is the predictable result of public choice incentives.
Recommended
Medical researcher Dr. Henry I. Miller, MS, MD described in his book his eye-opening time in the employ of the FDA: “when I headed the team at the FDA that was reviewing the NDA [application] for recombinant human insulin…my supervisor refused to sign off on the approval,” despite plenty of evidence that the drug was safe and effective in treating patients. His supervisor was concerned about the employment consequences should the FDA approve the product and a patient was harmed as a result. Product complications are always on full media display, and by all indications, the FDA would rather avoid the spotlight and quietly delay life-saving products.
Unfortunately, this problem is hardly limited to vaccines and insulin. A 2019 study by MIT researchers found that FDA standards are far too strict for medications geared toward severe diseases such as pancreatic cancer. An overly cautious bureaucracy demands complicated trials for medications that could help patients right away. Tufts Center for the Study of Drug Development deputy director Kenneth Getz writes that “the volume and diversity of data being collected is contributing to high levels of delays and inefficiencies,” and research protocols are becoming more complex, despite “high industry awareness in the adverse impact that protocol complexity has on clinical trial performance…”
It's of course critical that the FDA works with companies to investigate the evidence and determine the safety and efficacy of new medicines. However, unnecessary foot-dragging is unwelcome, especially when thousands of Americans are dying each day from COVID-19. Meanwhile, less stringent U.K. approval standards have hardly resulted in a flood of unsafe drugs unleashed on British patients. Surely, a vaccine deemed safe for U.K. patients should not be kept from patients on the other side of the pond. Let’s end the delay and quash this deadly disease once and for all.
Ross Marchand is a senior fellow for the Taxpayers Protection Alliance.






















Join the conversation as a VIP Member